Ankle Arthritis - Arthrodesis
Ankle arthritis is degeneration and eventual loss of the cartilage lining of the ankle joint. It leads to pain, swelling and stiffness (restricted movement) of the joint. It is commonly due to cartilage injury (trauma), but it can have other causes. Initial treatment is aimed at lessening the symptoms with conservative treatments. If these measures fail to control your symptoms, surgery is indicated. Ankle arthrodesis is an effective way to control the pain due to ankle arthritis. It does eliminate movement in the ankle joint, but other joints around the ankle compensate and allow up to 30% of pre-existing ‘up-down’ and ‘side-side’ motion. Most patients walk with a minimal or imperceptible limp.
The Surgery
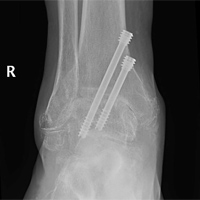
You will need to have a general anaesthetic. Antibiotics are administered intra-venously. The ankle joint is examined with a small camera (arthroscopy) through two ‘keyhole incisions’ at the front of the ankle. The remaining diseased cartilage is removed from the ankle joint surfaces and compression screws are used to hold the two bones together. Occasionally a larger incision has to be made to access the whole joint, apply a plate and screws or to allow correction of a significant deformity The skin is closed and a cast or boot is applied.
Post-Operatively
You will have your foot elevated on 1-2 pillows to reduce swelling. The local anaesthetic (block) will provide you with pain relief, but you may need to take medication as well. You will generally spend one night in hospital and you will be safe to ambulate on crutches as soon as you feel comfortable. You will be given intravenous antibiotics whilst in hospital. You will need to take medications for pain relief and for DVT prevention (Clexane injections or Aspirin) during your stay and upon discharge. The cast and sutures are removed at 2 weeks. The cast needs to remain dry and intact until your follow-up. Below is an estimate of your recovery.
- Activity
- Timeframe (approximate)
- No weight bearing in cast
- 0-6 wks
- Walking with boot and crutches
- 6-12wks
- Physiotherapy
- From 6wks
- Full Recovery
- 6 -12 mts
- Activity
- Time-frame
- Walking
- 6 weeks
- Driving (right ankle)
- 3 months
- Heavy Work
- 6 months
- Sport
- 12 months
Risks of surgery
All surgical procedures carry some risk. The risk of complications with ankle fusion low. Most patients benefit from surgery. A small number of patients can be made worse. You should weigh up the benefits with the risks prior to electing to have surgery.
This is a list of some of the problems which can occur:
- Infection – minimised with antibiotics, elevation, keeping the dressing clean and dry
- Wound healing problems – increased if smoking, diabetes, poor circulation
- Nerve injury – resulting in numbness or pins and needles, occasionally pain or muscle weakness
- Vascular injury – very rare, but may lead to compromised circulation and further surgery
- Swelling – is normal and improves with time, but can persist past 12 months
- Delayed union – fusion may be slow to occur, smoking is a significant risk factor
- Non-union – failure of the fusion to occur, smoking is a significant risk factor, may need re-operation
- Mal-union – resulting in persisting or new deformity of the ankle joint, may require further surgery
- Hardware related problems – loss of fixation prominent screw heads, broken screws rarely
- DVT/PE – clot in the deep veins of the leg or the lungs (increased if smoking or previous history)
- Complex regional pain syndrome (CRPS) – nerve pain syndrome, risk reduced with Vitamin C 500mg daily for 40 days
- Failure to relieve pain or transfer of pain to another part of foot
- Degeneration of adjacent joints – this universally occurs, however rarely needs further surgery
- Anaesthetic complications – more likely if there are pre-existing medical disorders (heart, lung, kidney)
You will need the Adobe Reader to view and print these documents.
![]()